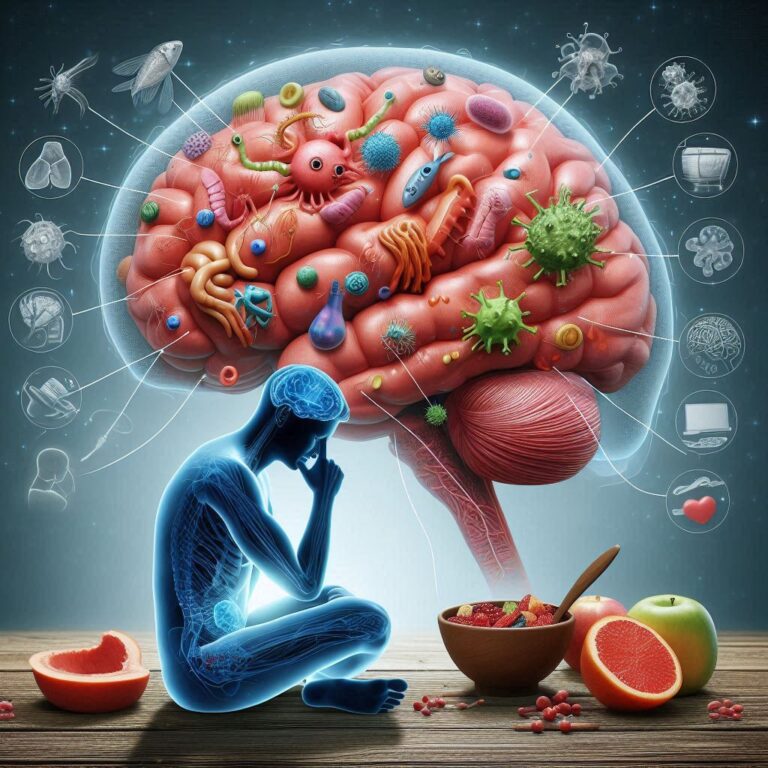
Gut-brain connection—Trillions of bacteria, sometimes called the gut flora, call the human stomach home and are vital for general health. Often known as the gut-brain connection, recent studies have revealed an intriguing relationship between mental health and gut condition. The gut-brain axis helps to coordinate this complex relationship—a bidirectional communication system including the endocrine, immunological, and neurological systems.
Essential for mood control, neurotransmitter synthesis, including serotonin and dopamine, is influenced by gut bacterial balance. Conditions including anxiety, depression, and even neurodegenerative illnesses have been connected to an imbalance sometimes referred to as dysbiosis. Gut bacteria can be changed by diet, stress, and antibiotics, influencing mental health. Knowing this link opens new directions for using dietary therapies, probiotics, and lifestyle modifications to address psychological problems. The effect of gut bacteria on mental health is investigated in this paper, and strategies are used to help maintain a better gut-brain balance.
The Science Driving the Gut-Brain Connection
The stomach and brain interact through several neurological, immunological, and endocrine channels. The vagus nerve, which connects the gut to the brain directly, is one prominent participant in this correspondence. This nerve allows impulses to move in both directions; hence, our mental state can be directly influenced by what happens in our stomach or vice versa.
The synthesis of neurotransmitters is yet another critical consideration. These are vital for controlling mood, stress reactions, and cognitive performance; the gut microbiota generates a good amount of serotonin, dopamine, and gamma-aminobutyric acid (GABA). Conditions like sadness, anxiety, and even neurodegenerative disorders like Alzheimer’s have been connected to imbalances in these neurotransmitters.
How Might Gut Bacteria Affect Anxiety and Mood?
Studies have indicated that dysbiosis—an imbalance of gut bacteria—may be a factor in mental health problems. People with anxiety and depression, for instance, might have less variation in their gut flora. Research using mice has shown that gut bacteria from sad people may cause depression-like symptoms when transplanted into healthy mice, therefore supporting the theory that gut health is very vital for mental well-being.
Anxiety and depressed feelings have been reported to be lowered by several types of bacteria, including Bifidobacterium and Lactobacillus. By helping to control inflammation, boost neurotransmitter synthesis, and strengthen gut lining integrity, these probiotic bacteria stop dangerous toxins from entering the circulation and set off an immune reaction that could compromise brain function.
How Diet Affects the Gut-Brain Axis
Diet profoundly shapes gut microbiota and, hence, mental health. Processed meals, too much sugar, synthetic sweeteners, and a lack of fibre can throw off gut bacteria’s balance and aggravate inflammation—a common link to mood problems. Conversely, a diet high in varied, complete foods can boost brain function and help maintain a good microbiota.
Foods Boosting Mental and Gut Health
- Yoghurt, kefir, kimchi, sauerkraut, and miso all have probiotics that boost serotonin synthesis and assist in preserving healthy gut flora.
- Prebiotic-Rich Foods: Garlic, onions, leeks, bananas, and asparagus abound in prebiotics, which feed helpful gut bacteria therefore fostering their development and activity.
- Omega-3 fatty acids, found in walnuts, flaxseeds, salmon, mackerel, sardines, and walnuts, contain anti-inflammatory qualities that improve brain function and lower symptoms of depression.
- Foods High in Polyphenol Richness Polyphenols found in berries, dark chocolate, green tea, and coffee have been demonstrated to favorably affect gut microbes and lower inflammation connected to stress.
- Whole grains, legumes, fruits, and vegetables help digestion and general gut health and add to microbial diversity.
- Bone broth and collagen help maintain gut lining integrity, lowering gut permeability (leaky gut) that may aggravate inflammation and psychological problems.

Environmental Elements Improving Gut-Brain Function
Beyond eating, various lifestyle choices support a good gut and enhanced mental health:
- Regular Exercise: Short-chain fatty acids (SCFAs), which improve brain function, have been demonstrated to be produced by physical activity, increasing gut bacterial diversity.
- Chronic stress changes the makeup of gut microorganisms and raises gut permeability, compromising gut health. Mindfulness, meditation, deep breathing, and yoga can better control stress.
- Enough sleep is essential, as bad sleep quality could upset the gut flora and aggravate mental problems. Making sleep hygiene a priority—keeping a regular sleep schedule and cutting screen time before bed—helps both gut and brain function.
- Avoiding Antibiotic Overuse: Although antibiotics are necessary to treat bacterial illnesses, too many can upset gut flora and cause dysbiosis. Probiotics should be taken whenever feasible to restore gut equilibrium after antibiotic use.
The Development of Gut-Brain Research
With a fresh understanding of mental health treatment provided by research on the gut-brain connection, this field has become somewhat active recently. Scientists are learning how gut bacteria affect cognitive health, mood control, and brain function. Probiotics and psychobiotics—specific strains of bacteria that can favorably affect mental health by altering neurotransmitter synthesis and lowering inflammation—have emerged from this developing discipline and
Fecal microbiota transplantation (FMT), in which healthy gut bacteria are moved from a donor to restore microbial balance, is another exciting option. Early research indicates that by enhancing gut health, FMT might help reduce symptoms of anxiety and sadness. Furthermore, tailored diets, depending on microbiome composition, are under investigation as a possible approach to mental well-being. These creative solutions could transform mental health therapy as gut-brain research develops by providing more focused and all-encompassing methods to control psychiatric conditions.
Conclusion
The gut-brain connection highlights the profound influence of gut bacteria on mental well-being. The trillions of microorganisms in our digestive system play a key role in regulating mood, stress levels, and cognitive function. An imbalance in gut microbiota, known as dysbiosis, has been linked to anxiety, depression, and neurodegenerative disorders. Fortunately, maintaining a healthy microbiome through lifestyle choices can support mental health.
A diet rich in fiber, fermented foods, and prebiotics nourishes beneficial bacteria, while regular physical activity enhances gut diversity and brain function. Stress management techniques like meditation and mindfulness also help regulate the gut-brain axis. Proper sleep hygiene is also essential, as sleep deprivation can disrupt gut bacteria and negatively impact mood. As scientific research continues to uncover the intricate relationship between gut health and mental well-being, adopting a holistic approach to diet, exercise, and stress reduction will be increasingly vital for maintaining a balanced mind and body.